The immune system is a complex system of tissues, cells, and organs that detects and acts against threats to your health.
The first layer of protection we have against infections is our skin – it provides a physical barrier between your organs and systems and bacteria, viruses, parasites and toxins you may encounter. We also have complex microbiomes – microorganisms that exist on our skin, in our mouths and noses, and in our guts. The microbiome can protect us from certain illnesses. Finally, there are cells generated by the immune system (white blood cells like T-cells, B-cells, macrophages and others) and proteins (antibodies, cytokines and others).
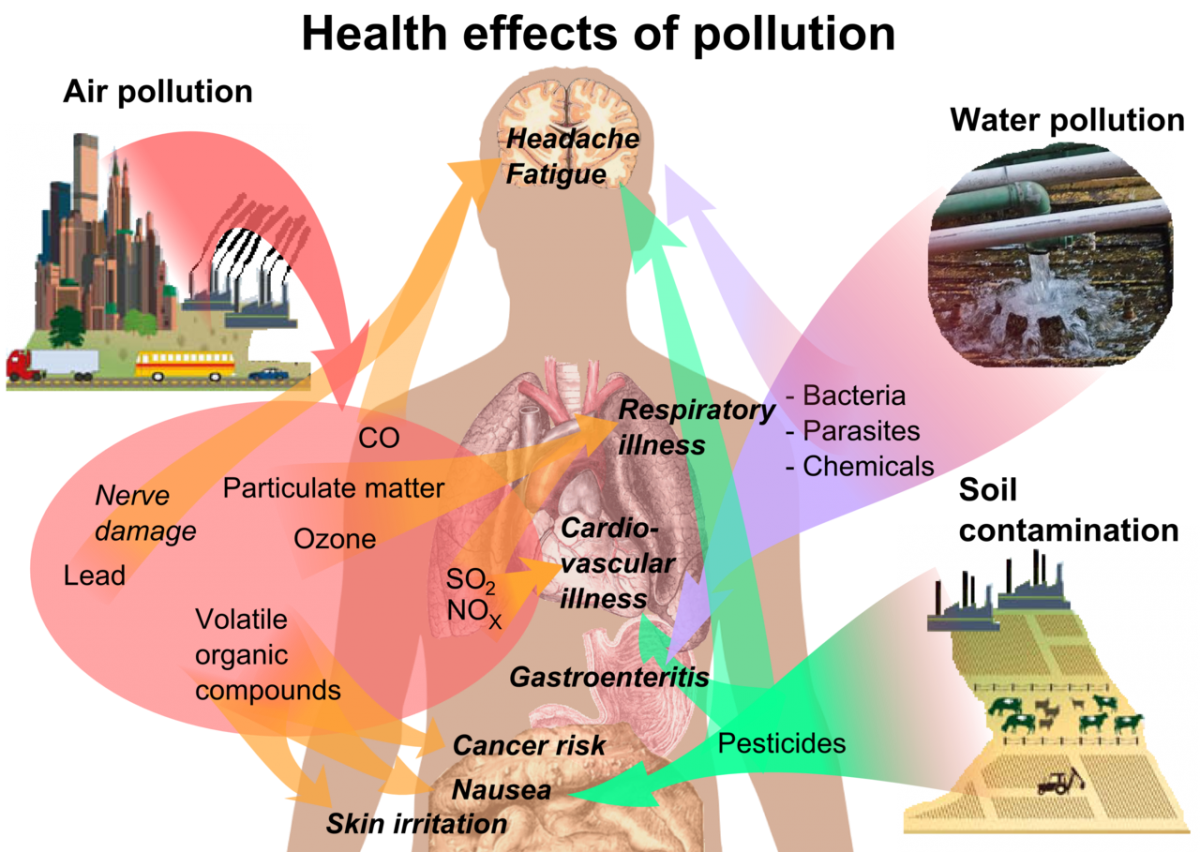
Can you boost your immune system? Because it is quite complex, scientists are still unraveling all of the connections between our lifestyles and immune function. We do know there are certain behaviors that can help protect us from disease – avoiding exposures to chemicals like tobacco smoke, washing our hands, and others – https://www.health.harvard.edu/staying-healthy/how-to-boost-your-immune-system.
Microorganisms that can make us sick are called pathogens – https://www.mayoclinic.org/diseases-conditions/infectious-diseases/in-depth/germs/art-20045289. Sometimes they live on and in our bodies without causing illness. Other times, they can multiply to the levels of causing disease.
SARS-CoV-2 is the virus that can cause COVID-19, the respiratory illness that is now pandemic. This is a novel virus, but it is related to other coronaviruses that sometimes cause seasonal colds, and have caused 2 other epidemics in the last two decades – SARS and MERS. Viruses are pieces of genetic material encased in a shell with binding proteins. They enter the body and invade our own cells in order to make copies of themselves. The below video gives a short explanation of how the coronavirus functions, but was made in March 2020, so does not contain up-to-date information on the pandemic.
The COVID-19 pandemic began at the end of 2019. It is a respiratory disease that has a relatively long incubation period (the period of time people don’t have symptoms even if they are infected), can spread even when people don’t have symptoms, seems to mainly spread through droplet and direct contact exposure, and can cause severe illness and death in some people. Find more detailed information here – https://www.cdc.gov/coronavirus/2019-nCoV/index.html
More information on SARS-CoV-2 variants is explained here:
Late in 2020, several vaccines for SARS-CoV-2 have been developed and 3 have been approved for use in the United States (with several others being used in other countries). Vaccines generally work by teaching your immune system to create antibodies which can attack the pathogen when you come in contact with it. There are two vaccines that have been approved by the FDA currently are both based on the mRNA or messenger RNA molecule. These molecules instruct your cells to make a protein on the surface of SARS-CoV-2 (the spike protein), which your immune system recognizes as a foreign body and begins to manufacture antibodies. Another vaccine made by J & J works by introducing another harmless virus (adenovirus) in order to bring pieces of SARS-CoV-2 to your immune system. Read more about the current vaccine research here https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines
In 2022, vaccines have been approved for most age groups, we have had booster shots, wide-spread testing became possible, and treatments for COVID-19 have improved a lot. However, variants have continued to spread and have become more contagious and mitigation policies have mostly disappeared. We’ve understood the disease more and people continue to get sick and even die, but people and governments have mostly returned back to the lives we led before the pandemic started. People can still be more vulnerable to the disease, especially those who are immuno-compromised in some way, people who are getting treated for cancer, people living with chronic diseases, and others. An important issue for all is that a considerable percentage of people who get sick with COVID-19 can develop long-term symptoms, some debilitating. It is unfortunate that mitigation measures are no longer required and this disease is establishing itself as something we will continue to struggle with for years to come.