Conventional medical and health care are also called allopathic or Western medicine. This is in contrast with complementary, alternative, or integrative health approaches. Most of the healthcare you have probably gotten in the United States is this type of care – the kind where doctors, nurses and other affiliated medical professionals provide the care.
This type of care generally concerns itself with diagnosing, preventing and treating disease. Disease or illness in this system of care is thought to happen because of organic changes in the body, like atherosclerosis, or from exposure to pathogens like bacteria and viruses.
The people who provide conventional care are medical doctors who hold MD or DO degrees, nurses (who may have a bachelor’s or master’s degree and who are licensed as RNs or NPs), physical therapists, and various other allied medical professionals. Examples include emergency medical technicians (EMTs), respiratory therapists, dentists, podiatrists, optometrists, and others.
Most medical doctors hold the MD (medical doctor) degree, and some may also have a DO or Doctor of Osteopathy degree. They attend accredited medical schools for several years, then have periods of residency and internship, and some may choose to specialize further. Doctors who provide general every-day medical care are usually those who studied internal medicine or family medicine. They may be known as general practitioners or primary care providers. They can see people for common complaints like respiratory infections, and well-care (check-ups that may include blood laboratories, blood pressure screenings, vaccines, and other prevention and routine care). They can order screening tests, blood work, medical imaging like X-rays or MRIs, and other diagnostic tools, and can prescribe medications. Doctors’ offices may also have Nurse Practitioners (NP) or Physician Assistants (PA) provide this kind of care under the supervision of the doctor.
Doctors who choose to specialize, spend several more years working in a particular area of medicine. This can be based on a particular body system, like cardiology or neurology, a kind of patient, like pediatrics or gynecology/obstetrics, or particular type of disease, like oncology (specializing in cancers). Usually, a primary care provider may refer their patient to a specialist if they require more than routine every-day care.
Conventional care is also found in hospitals, urgent care centers, and rehabilitation centers. Here, many allied health professionals may be present to help doctors provide care.
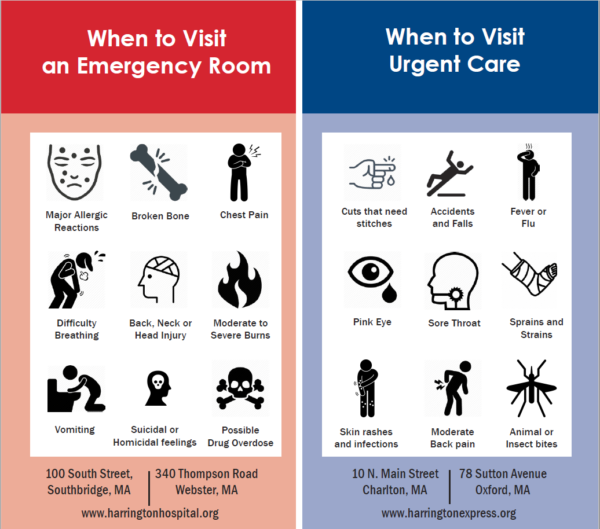
When should you seek emergency care and when should you go to an urgent care center? Generally, you should go to the emergency room for a life-threatening condition (heart attack), sudden serious changes like shortness of breath, numbness or paralysis, or serious/severe conditions like trauma, severe cuts or burns, severe allergic reactions and so on. Urgent care is for times when you need care right away and may not be able to see your primary provider quickly – things like respiratory infections, earaches, etc. Get your preventative care from your primary care provider.